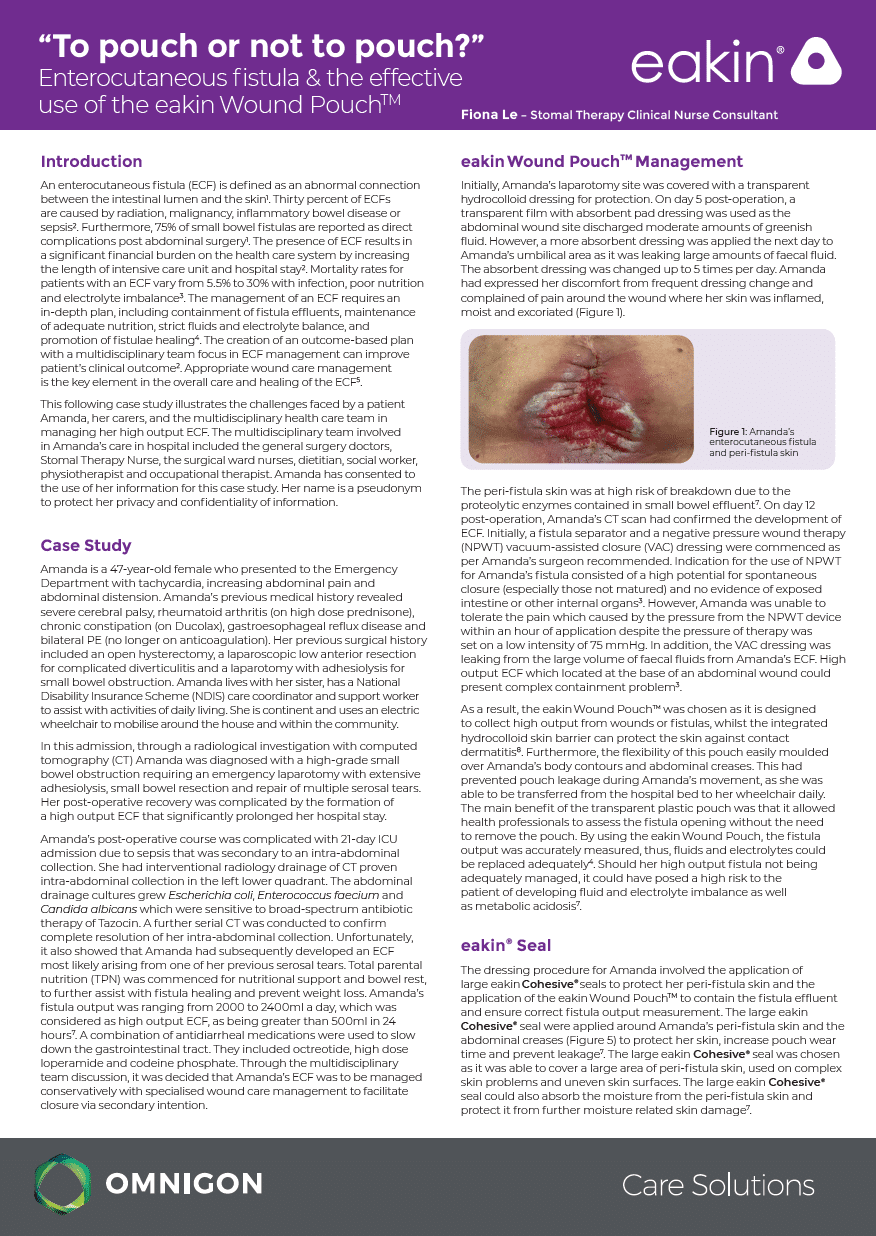
An enterocutaneous fistula (ECF) is defined as an abnormal connection between the intestinal lumen and the skin1. Thirty percent of ECFs are caused by radiation, malignancy, inflammatory bowel disease or sepsis. Furthermore, 75% of small bowel fistulas are reported as direct complications post abdominal surgery. The presence of ECF results in a significant financial burden on the health care system by increasing the length of intensive care unit and hospital stay2. Mortality rates for patients with an ECF vary from 5.5% to 30% with infection, poor nutrition and electrolyte imbalance3. The management of an ECF requires an in-depth plan, including containment of fistula effluents, maintenance of adequate nutrition, strict fluids and electrolyte balance, and promotion of fistulae healing4. The creation of an outcome-based plan with a multidisciplinary team focus in ECF management can improve patient’s clinical outcome2. Appropriate wound care management is the key element in the overall care and healing of the ECF5.
This following case study illustrates the challenges faced by a patient Amanda, her carers, and the multidisciplinary health care team in managing her high output ECF. The multidisciplinary team involved in Amanda’s care in hospital included the general surgery doctors, Stomal Therapy Nurse, the surgical ward nurses, dietitian, social worker, physiotherapist and occupational therapist. Amanda has consented to the use of her information for this case study. Her name is a pseudonym to protect her privacy and confidentiality of information.
Download the case study to continue reading.
Download